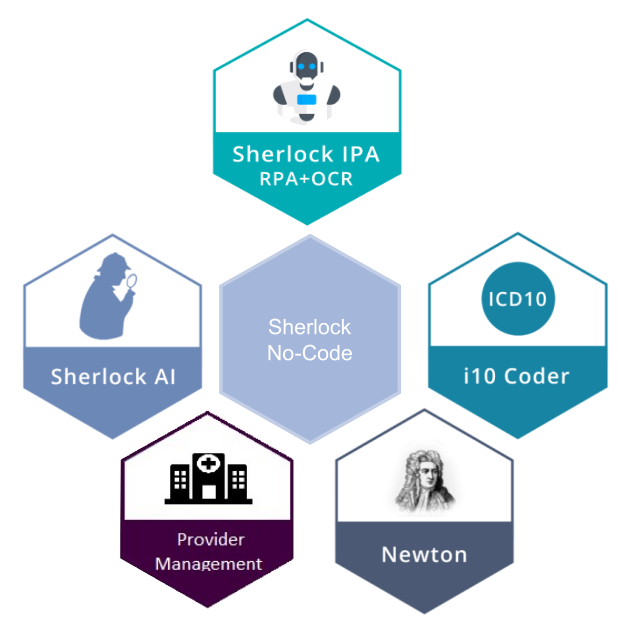
Sherlock Suite for Global Payers
Sherlock Suite is a state-of-the-art AI native platform for digitizing and automating medical claim processing, stopping leakages and fighting fraud & abuse.
Technologies
SaaS
Sherlock is a Software as a Service platform and works on the most secure cloud infrastructure. It is provided in a Highly Available manner to allow your business to function without interruptions
Micro Services
Sherlock’s underlying design is based on a Micro-Services Architecture. Resulting high architectural flexibility allows Sherlock to rapidly deploy newer innovations and always help you stay ahead of the curve
Simple Integration
Sherlock’s simple APIs allow easy integration with your internal systems and works in a near plug-and-play fashion. The integration and go-live time could be as little as one week to a maximum of twelve weeks, so you can start deriving the RoI rapidly.
Visualizations
Sherlock provides incredible insights and data visualizations. These visualizations help the business teams further feedback interesting insights in product design and delivery, thereby compounding benefits of the platform
Sherlock.IPA
Sherlock Intelligent Process Automation suite combines features of Robotic Process Automation and OCR at 99%+ accuracy to help churn the complete medical and financial information from incoming claim documentation. The rich information allows for smooth and Touch-Free-Claims™ processing, utilizing clinical, financial, policy and business knowledge acquired over processing millions of claims.
Sherlock.IPA is our state-of-the-art platform for claim digitalization and automation. Sherlock.IPA takes incoming claim documents from multiple sources, performs an OCR process on the document performing the following actions:
Features
Auto pickup claim scanned documents/ pdfs from a folder and process them.
Document classification and missing document identification
Digitizing Consolidated Bill, mapping claim lines to standard field names
Digitizing Discharge Summaries and Flagging Potential PEDs by sifting through the document
Auto ICD Coding, including primary and secondary codes, using integration with Sherlock.i10Coder
Capturing textual fields to enable subsequent text analytics
Digitizing Detailed Bill and Flagging Non-Payables
Integrating with Sherlock.AI and automate final decision
Sherlock.i10Coder
Sherlock.i10Coder picks up diagnosis information captured from the Discharge Summary and provides required ICD 10 codes.
Sherlock.i10Coder is a multi-tenant SaaS platform, hosted on Perceptiviti cloud. Sherlock.i10coder stores no PHI or PII to ensure data protection and security.
Sherlock.AI
Once the information is churned from the claim documentation and converted to structured information, Sherlock.AI brings in advanced machine learning models to provide a Risk Score each incoming claims. Thereby helping flag claims that do not adhere to policy or clinical norms as well as clearing claims that are clean. Sherlock.AI helps insurers significantly improve savings by cutting claim leakages, while improve processing efficiency by identifying clean claims
Sherlock.AI is a Claim Auto-Adjudication platform. Sherlock.AI uses the digitize claim data as well as policy and member data and runs it through the following algorithms:
Features
Proprietary AI/ML algorithms to arrive at a decision to pay or deny the claim
Cognitive ruleset to assess Claim Eligibility: Compliance with policy in-force conditions, dates, Member enrolment conditions, member relationship eligibility conditions
Cognitive ruleset to assess Claim Admissibility: Compliance with guidelines, availability of sufficient documents to process, Discrepancy checks
Cognitive ruleset to assess Claim Applicability: Waiting period applicability, PED applicability, SI enhancement, Portability and SI Enhancement waiting period applicability
Cognitive ruleset to assess Estimated Amount: Over a period of time, the system can also start predicting approximate “approvable” amounts for each claim
Provider Management Platform
Effective Provider Network Management using insight and analytics driven by massive data available to the payers is a key success factor.
Perceptiviti’s Provider Management Platform allows payers to effectively manage and maximize the return from their provider relations.
Features
Consolidate Provider data from multiple source systems, including the claims system, contracts and tariffs, PBM, provider portals and provider licensing data into a Single-Source-of-Truth data mart.
Generate provider specific 360 degree insights and analytics
Compare multiple providers against each other
Create action plans, follow through to completion
Provider CRM features including task and action tracking
Provider facing workflows
Enable cross team collaboration among Network Management, Claims, Underwriting and Audit teams that interact with the providers.
Sherlock Analytics AI
Sherlock Analytics AI is the Claims business intelligence for Payers. It provides MIS and KPI tracking for all the parameters important for a Payer, including regulatory reports.
Features
Overall Claim Summary Dashboards
Disease Level Reports
Provider/ Hospital Level Reports
Demographic Reports
Ad-hoc User Generated Reports
Professional Services
Perceptiviti professional services provides product engineering, AI/ML, data sciences and cloud services to our customers across the globe. Our current clients include some of the largest enterprises globally.
Digitization
Digital transformation of various business processes, using proprietary or third party digitization tools.
AI/ML Services
- Computer Vision,
- Natural Language Processing,
- Risk Profiling Predictions
Big Data & Data Warehousing
- Data Management Data Collation,
- Aggregation & Cleansing Data Platform
Advanced Analytics & Reporting
- Advanced Analytics & Management,
- Reporting Customer Profiling
Underwriting Automation for Insurers
- Health,
- Life Motor